Minimally Invasive Aortic Surgery
Aortic Aneurysm
The aorta is the largest artery in your body and runs from your heart, down through your chest and into the abdomen. It the divides into two blood vessels called the left and right common iliac arteries. An aortic aneurysm occurs when the wall of the aorta progressively weakens and begins to bulge. An aortic aneurysm may continue to enlarge and eventually rupture if left untreated, causing severe internal bleeding and possibly death.
Unfortunately most aortic aneurysms are never detected. That is because more than 80% of patients are asymptomatic - that they experience no symptoms at all and don't know they are living with an aortic aneurysm. In fact most aortic aneurysms are discovered inadvertently during procedures to diagnose other conditions such as an abdominal ultrasound or CT scan or a chest x- ray examination. It is important to discover aortic aneurysms because they are a leading cause of death amongst those over the age of 60. Many of these deaths are preventable if the aneurysm can be detected and safely treated prior to the aneurysm rupturing.
Aortic aneurysms are more common in those over the age of 60 especially if they have ever smoked cigarettes or have someone in the family who had an aneurysm. The can occur in both men and women but are more common in men. The majority of aneurysms occur as a result of a genetic predisposition to aortic dilatation coupled with various insults such as smoking or high blood pressure.
In some people aortic aneurysms can cause symptoms such as pain or a pulsing feeling. The location of this can vary with the location of the aneurysm - upper back, lower back or abdominal pain or discomfort.
How is an aortic aneurysm diagnosed?
Screening tests used to detect an aortic aneurysm include a chest x-ray and an abdominal ultrasound scan. Once the aneurysm has been detected a more detailed imaging investigation such as a CT scan with intravenous contrast may be requested depending on the predicted size of the aneurysm and the patients' renal function and any previous reactions to radio-contrast dye. The CT scan is also the best investigation before deciding if treatment is necessary and in designing a stentgraft that will fit the patients' individual aortic anatomy.

Figure1
Figure 1 shows a high quality CT scan of the abdomen and pelvis. This patient has a juxtarenal aortic aneurysm that is clearly visible on this 3D reconstructed image from a CT workstation.
Who should be tested to see if they have an aortic aneurysm?
The following groups should have an abdominal ultrasound performed to check for an aortic aneurysm:
- Men aged >50 who have smoked at least 100 cigarettes during their life
- Men and women aged >50 with a family history of AAA
- Men and women aged >60 with a history of TIA or stroke
- Men and women aged >60 with a history of CABG
Should I be worried?
Aortic aneurysms can be safely treated or cured with early diagnosis. The key is to diagnose the aneurysm before it has ruptured so as to plan an elective minimally invasive repair. At Specialist Vascular Clinic we have extensive experience with minimally invasive endovascular stentgraft treatment for all types of aortic aneurysms. In screening for this condition we have the opportunity to save thousands of lives.
What should I do if I have an aortic aneurysm?
Contact Specialist Vascular Clinic. You will be seen by a leading vascular and endovascular surgeon who has undertaken specific subspecialty training in this field and has extensive experience in the modern management of aortic aneurysms. All the treatment options will be discussed with you at length. The optimal management plan will be tailored to your individual condition and only then can you be assured of receiving the care that is most appropriate.
What is minimally invasive aortic surgery?
Minimally invasive aortic surgery involves using endovascular techniques to place stentgrafts within the aortic lumen to divert blood flow away from the aneurysm sac. There is a reduction in perioperative mortality compared to standard open surgical aneurysm therapies.
Most abdominal aortic aneurysms (AAAs) and many thoracic aortic aneurysms (TAA) can now be repaired completely percutaneously using endovascular stentgrafts without the need for any incisions or wounds. This minimally invasive procedure is performed via a needle in each groin and can be safely performed under general, regional or local anaesthesia depending on the patients' preferences and co morbidities.
When an aortic aneurysm repair is being planned we use sophisticated spiral CT scan technology together with a 3D workstation to help plan a customised stentgraft that is designed to fit the patients' particular aortic anatomy. This modular type of stentgraft design allows each component of the repair to fit precisely into the aorta as intended in order to seal off the patients aneurysm from pulsatile blood flow.
The endovascular stentgrafts are usually introduced from the femoral arteries in the groins. Once accessed via a needle, a guide wire can be placed inside the aorta and the stentgrafts are telescoped over the wire and thus introduced into the patients' aneurysm. Once in the correct position as confirmed by angiography, the devices are opened in a controlled fashion ensuring precise anatomical deployment. At the conclusion, the previously inserted closure device is used to close the entry site in the femoral arteries which allows the entire procedure to be performed without incisions or wounds. This has significant advantages for the patient who can rapidly resume normal activities following the procedure. This has led to significant reductions in hospital length of stay, time to resume ambulation, time to return to normal pre-admission activities.
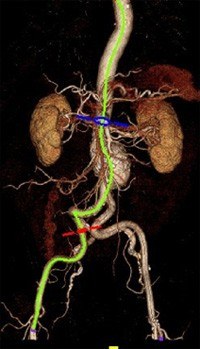
Figure 2
Figure 2 shows a typical CT scan appearance of an AAA as a bulge or dilatation of the aorta just below the level of the kidneys and just above the level of the aortic bifurcation. The green line is a centreline of flow analysis being performed to help plan the construction of an endograft that will allow an endovascular repair. This line is also the line that the device will follow when introduced from the femoral artery and deployed in the aorta.

Figure 3
Figure 3 shows a typical appearance of an AAA at angiography. This is the view of the aneurysm the surgeon works with during the endovascular procedure to repair the aneurysm.
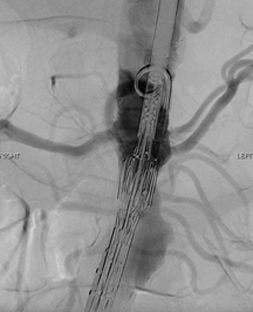
Figure 4
Figure 4 shows the endovascular stentgraft in the correct position and being deployed during the implantation procedure.

Figure 5
Figure 5 reveals the completed angiographic appearance of a successful endovascular AAA repair with excellent flow in all the renal arteries as well as all the iliac arteries and with no blood flow in the aortic aneurysm. The aneurysm sac has now been excluded from the arterial circulation and is monitored in follow up as it shrinks in size.
What if my doctor said my aneurysm was not suitable for a stent?
There are no absolute anatomical restrictions on performing an endovascular repair with stentgrafts. Aneurysms in previous years considered not suitable for stenting can now be treated because of advancements in the technology that allow the treatment of the most complex of aneurysms. Today, there are no true contraindications to endovascular repair; instead it is the risk/benefit ratio of each possible treatment option that must be considered for individual patients.
Specialist Vascular Clinic is one of a few centres around the world able to offer patients a pure endovascular repair for complex aortic diseases such as juxtarenal, suprarenal, thoracoabdominal and aortic arch aneurysms. These complex aortic pathologies require a more specialised level of surgery which is ideally offered by surgeons who have undertaken subspecialty training in this area of vascular and endovascular surgery.
Endovascular therapy using commercially available stentgrafts is frequently utilized to treat infrarenal abdominal aortic aneurysms (AAA). Large randomized trials have shown this minimally invasive technique to reduce the mortality rate associated with repair from ~5% with open surgery to ~1% with endovascular aneurysm repair (EVAR). However, when the aortic repair involves the renal arteries or the visceral segment of the aorta, operative risks for open surgical repair are significantly higher with mortality rates of 10-30%. There are also more risks to consider including risks of renal ischaemic time leading to renal failure, bowel and hepatic ischaemia, as well as paralysis from spinal cord ischaemia. These risks are highest for patients that present with thoracoabdominal aortic aneurysms (TAAA).
Operative results for open repair of TAAA correlate with surgical volume of both the individual surgeon as well as the institution. In high volume open surgical centres in the USA, mortality rates range from 10-15%. However, when the results all centres are pooled, the surgical outcomes are much more sobering. A recent state wide audit in the US state of California showed open TAAA had a perioperative 30 day mortality rate of 19% and at 1 year post repair only 69% of all patients were still alive.
Thus, it is this group of patients with more complex aortic disease associated with very high perioperative morbidity and mortality from conventional open surgery that will derive the greatest benefit from endovascular therapy. Endovascular therapy has the potential to not only reduce the morbidity and mortality of aortic repair but also allows treatment of a large group of patients that were previously considered 'inoperable' or 'too high a risk'.
Several centres from the United States and Europe have already reported promising early as well as midterm outcomes from this form of therapy for complex aortic disease. At the highest volume centre for endovascular therapy for complex aortic disease, the Cleveland Clinic, in Ohio where Dr Mohabbat completed his sub specialty training, greater than 1200 aortic aneurysms are repaired annually. They began treating juxtarenal AAAs with fenestrated stent grafts in 1999 and have published midterm follow up data on their patients. Their results demonstrate that juxtarenal AAAs can be repaired with a mortality rate of < 3% at and TAAAs can be repaired with a mortality rate of < 10%. In follow-up the device is stable, the vast majority of patients aneurysms continue to reduce in diameter, and renal and visceral complications are uncommon.
However it also clear that the intricacy and degree of complexity of designing and then implanting an aortic stent graft with branches to the coeliac, SMA, and renal arteries in the visceral segment or the subclavian and carotid arteries in the arch is several orders of magnitude higher than for infrarenal devices. Critical end organs depend on flow through the endoprosthesis being implanted and there is the potential for fatal complications. Thus the implanting surgeon is required to have specific subspecialty training in this field and should be proficient with planning, sizing, technical issues with implantation of aortic endografts, visceral and brachiocephalic artery stenting, and in troubleshooting for branched stentgrafts designs.
Today, there are no true contraindications to endovascular repair; instead it is the risk/benefit ratio of each possible treatment option that must be considered for individual patients. Patients with complex aortic disease have the most to gain from endovascular solutions. Surgeons who desire to implement these new technologies should ideally have subspecialty training in this field and be proficient with image interpretation, manipulation, endovascular grafting of the infrarenal aorta, and renal and mesenteric stenting prior to embarking on complex aortic procedures. Devices will become more complex and will be mated with additional small vessel stent grafts. However, clearly, the benefits of these technologies for this patient population are marked, and physicians must place great emphasis on the support of these technological developments and methods by which these skills can be disseminated.

Figure 6
Figure 6 demonstrates an aortic aneurysm that was previously considered not suitable for stents - juxtarenal, angulated neck, severe right renal artery stenosis. At Specialist Vascular Clinic this was successfully treated with a fenestrated stentgraft design incorporating branches for the left and right renal arteries as well as a branch for the Superior Mesenteric Artery (SMA). The scan demonstrates excellent flow through the stentgraft and its branches. There is no further filling of the aneurysm.